Reflections on the GMHC
This year’s Global Missions Health Conference was a special one. After a full two years, we were back in person. We got through some of the hardest days of our lives in 2020, and wasn’t it good to be together again in 2021? It felt like a family reunion, a time to gather together and remember all the ways that the Lord has been so faithful to us over the last two years.
I’m going to go over some highlights that stood out to me, but I would also encourage you to talk with your family and friends about what impacted you. Don’t just let this year’s conference come and go. Take that next step in missions. Talk, pray, learn, grow, listen. And if you weren’t at the conference this year, be encouraged by the 2200 people that were in person and online being challenged to enter into the next step of healthcare missions for the glory of God.
Arriving at the GMHC

As the conference is getting started each year, there is always a buzz of excitement in the air that you can almost feel. Exhibitors are setting up their booths, pre-conference meetings are happening, the registration counter is priming for thousands of people to arrive. The anticipation was even greater this year after our virtual only event in 2021.
As attendees, exhibitors, speakers, and volunteers started arriving on Thursday afternoon, masks were in place, but that did not diminish the joy in seeing one another in person and catching up on all that the has happened over the last few years. This year’s Thursday afternoon plenary with Dr. Daisey Dowell was an inspiring way to kick off the weekend. She challenged each one of us with her story and her perseverance and reminded us that we are all servants in training. New to this year’s conference was the addition of a Thursday evening church service with Southeast Christian Church. It gave attendees the chance to join in a worship service or take the time to visit exhibitors and learn more about what is happening in the world of healthcare missions.
Breakout Sessions

The breakout sessions were outstanding this year, with topics ranging from Domestic Health Disparities to International Equipping and everything in between. We had speakers from all over the globe, some even joining us via Zoom from the Middle East or Africa. Everyone had patience with this new digital world we live in, knowing that we have to be patient with technology sometimes! This was our first year to live stream some of our sessions and it was overall a great experience.
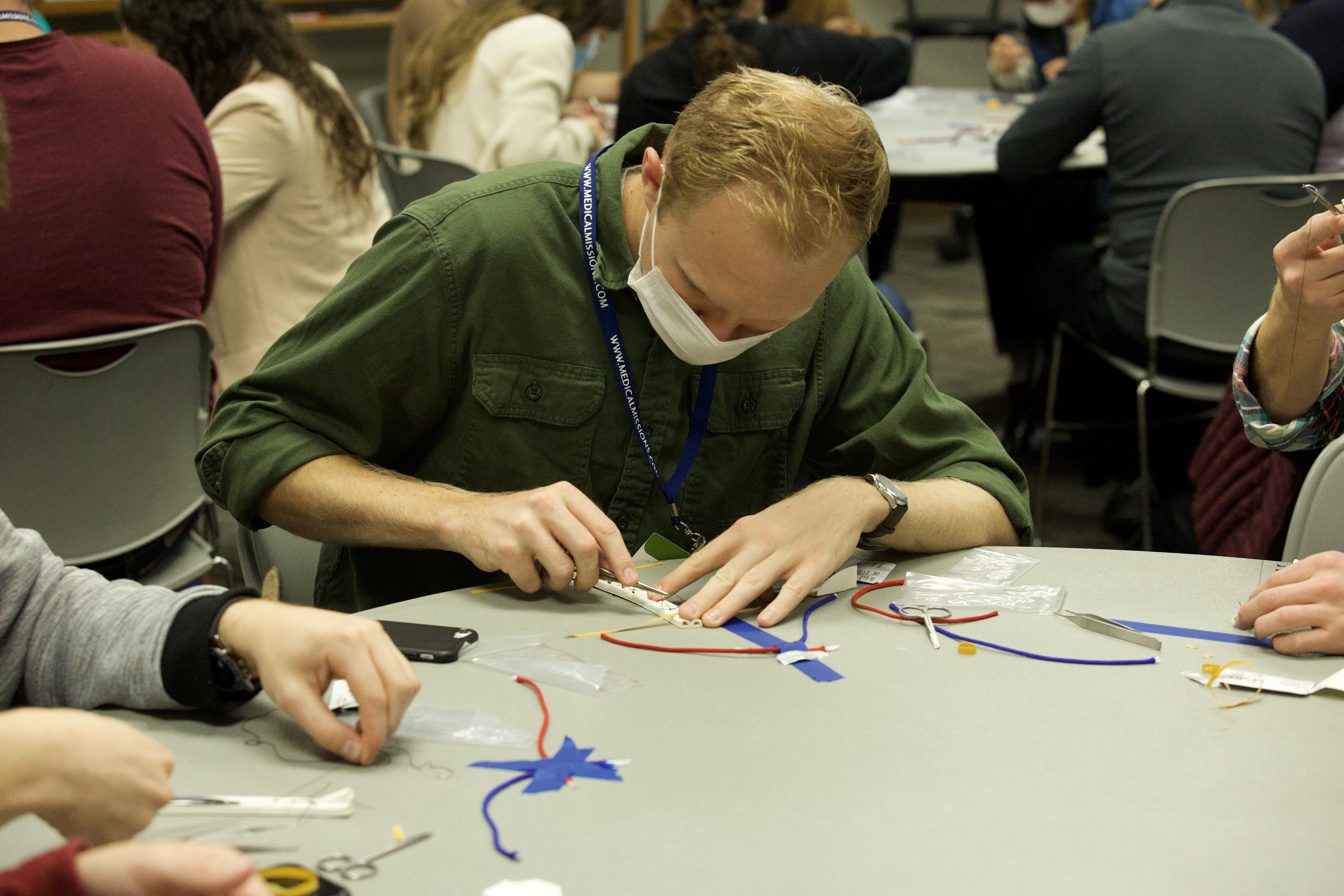
Our Hands On sessions were popular as always. Everyone loves learning how to suture, do an ultrasound with minimal equipment/skills, and equipping themselves with newborn care at birth. These hands-on sessions are a great way for our undergraduate students to get a taste of what could be their future!
Plenary Sessions

All of our plenary sessions this year were outstanding. On Friday Dr. Phil, Dr. Lee, and Dr. Hillis shared about how we can use data to make informed, loving decisions for those around us. On Friday we heard from many different speakers from all different backgrounds about their journeys in and through healthcare missions. Dr. Donlon was an amazing facilitator throughout that plenary and led us through the many ways that we can all be challenged to learn, pray, send, and go. On Saturday morning, Dr. Jason closed us out with a convicting talk on Z groups – the places and people in the world that have zero disciples. He called on us all to lay down on pride and our sense of self-importance in order to truly listen to Jesus’ call on our life. And we finished our time together with a call to commitment, in the traditional GMHC way – bringing a commitment card up to the map and laying it on a location we feel that God is pulling us toward. These cards will be mailed to everyone in a few months as a reminder of this time and this passion.
Other Fun and Interesting Tidbits

We tried out food trucks this year! The people who were in the front of the lines enjoyed the food trucks immensely…and the people in the back of the lines, not so much! While we know that some of you loved it and some of you didn’t, we are always committed to trying and improving. We’ll be back next year with something even better!
Our exhibitors were amazing as always. The exhibitors represent all the ways you can move toward your next step in missions, so their presence is extremely important to us. We are thrilled that so many exhibitors come ready to engage attendees with interactive and thoughtful displays and materials.
Our virtual audience was able to experience some unique interviews with speakers, exhibitors, and partners. This feature was a great way to go a little deeper and learn a little more about some of our most seasoned and experienced medical professionals. Many of them have been coming to the GMHC for years now, and they bring a wealth of knowledge. We’re lucky to have these amazing men and women in our midst!
We introduced a new idea that will be percolating for all of 2022 – the Pathways to Healthcare Missions. This idea was introduced in the Friday night plenary and we encouraged attendees to take the online survey so that we can tailor the forthcoming classes, materials, and online resources to your needs. We want to create resources that will be a guide and a pathway to help people navigate their next step, wherever that might be. We’re excited for where this path is going to take us!
Thank you.

Thank you for being a part of the GMHC. Whether you attended in person, virtually, or historically (or if you simply hope to attend someday!), we are thankful for you. We are thankful for your heart that desires to serve and for your skills that you are willing to share. You are an inspiration to us here at GMHC/MedicalMissions.com and you are the reason we do what we do. We long to see every people group and every nation experience the love of Jesus and the physical care that they deserve – and we hope that we can be a small part of you becoming the hands and feet of Jesus.
Related Content





Comments